For many specialties, working nights is an inevitable part of being a physician. The burden that comes with that schedule are well-established: disrupted sleep, social isolation, and the strain on both personal health and relationships. But what’s often overlooked is whether those trade-offs are compensated in a way that reflects their cost.
In this blog post, we analyzed more than 12,000 anonymous physician salary submissions on Marit to dive into the details. We looked at how common night work is across different specialties, how often it’s actually associated with higher pay, and what factors seem to drive the so-called “nocturnist premium”. The results show that while night work is widespread, the compensation for them is anything but consistent.
Night Work Is Everywhere, and Not Just for the Usual Suspects
In some specialties, night work is simply built into the job. On Marit, 95% of Emergency Medicine physicians report working nights. Critical Care is similar at 83%, and Neurosurgery (75%) and Surgery (72%) are not far behind. Even in Anesthesiology, where a lot of work is scheduled during the day, more than two-thirds of physicians report working nights.
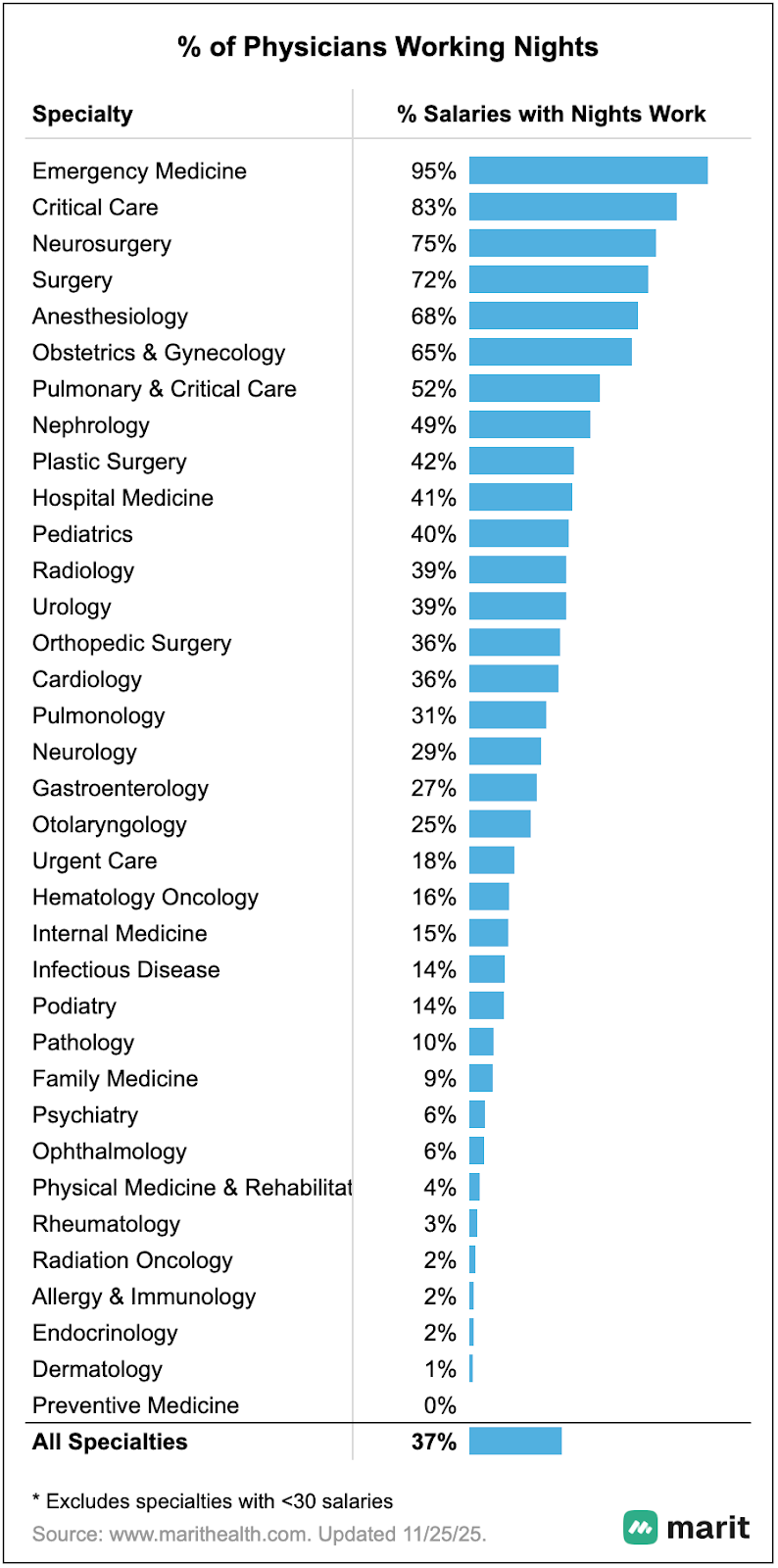
What may be more surprising is how often night work shows up in specialties that are usually perceived as more daytime-focused. Around 40% of Pediatricians report working nights, as do nearly 40% of Urologists and Radiologists. And even in Orthopedic Surgery, often thought of as more elective with mostly daytime schedules, more than a third of physicians have overnight work.
Taken together, the data makes one thing clear. Night work is not rare or limited to a few narrow roles - it’s a structural part of clinical practice across a wide range of specialties.
Where Working Nights Pays Off
When we compare total compensation for physicians who work nights with those who work daytime-only schedules, the size of the premium depends heavily on how night work functions within a given specialty.
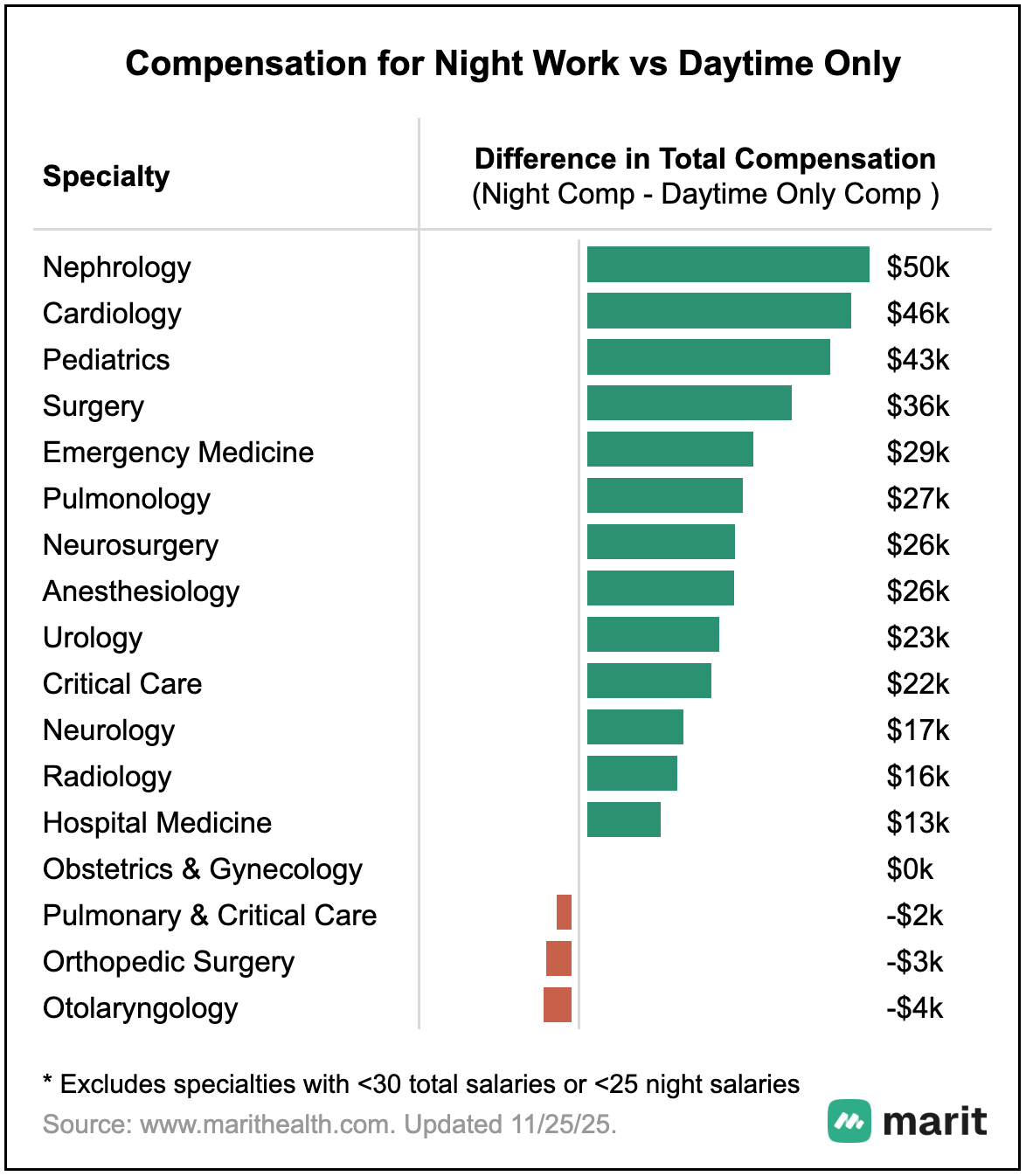
In Nephrology and Cardiology, physicians who work nights earn roughly $45,000 to $50,000 more per year than their daytime-only peers. In these specialties, night coverage is often discrete, harder to staff, and less easily absorbed into daytime workflows, which makes it more likely to be priced explicitly rather than quietly bundled into base compensation.
Pediatrics and Surgery fall into a similar, though slightly less uniform, category. Pediatricians who work nights earn about $40,000 more annually, while surgeons see a premium closer to $35,000. In both cases, night work is common but not universally shared, and is often handled through specific shifts, call structures, or roles rather than evenly distributed across all physicians. That separation appears to preserve a moderate premium.
Emergency Medicine still shows a meaningful premium, with physicians who report working nights earning roughly $30,000 more per year than those who report working days only. This likely reflects role differentiation within the specialty rather than night work being explicitly rewarded, such as distinct day-only roles that are tied to specific sites or leadership positions. These roles tend to trade higher compensation for less disruptive schedules.
Where the Premium Shrinks or Disappears
In other specialties, the financial upside of night work is far more limited. In Hospital Medicine, physicians who report working nights earn about $13,000 more than those who work daytime-only schedules. Radiology shows a slightly larger difference at roughly $16,000, while Neurology sits closer to $17,000. These gaps are real, but modest, especially when weighed against the cumulative disruption that night work creates. In these fields, overnight coverage is often integrated into standard schedules or shared broadly across groups, which can make it harder to isolate and price separately.
In a few specialties, the night work premium disappears altogether. In Obstetrics and Gynecology, total compensation is essentially unchanged whether physicians work nights or not. In Orthopedic Surgery and Otolaryngology, working nights is actually associated with slightly lower total compensation in the aggregate data. Rather than reflecting differences in workload or difficulty, this pattern points to compensation structures where overnight coverage is absorbed into baseline expectations, while higher total pay is more closely tied to daytime productivity, elective volume, or leadership responsibilities.
What This Means for Physicians
The real question isn’t whether working nights is “worth it” in general. It is whether your specific role, employer, and compensation model actually pays for it.
Two physicians in the same specialty can both work nights and experience very different outcomes depending on whether night shifts are optional or mandatory, whether they are paid separately or folded into base salary, and whether productivity metrics account for overnight work.
Before signing a contract that includes night coverage, it’s worth getting specific. How often are nights scheduled, and are they evenly distributed across the group? Are nights compensated separately or as part of the base salary? Does overnight work count toward productivity targets or incentive calculations?
Working nights may be unavoidable in some cases, but appropriate compensation isn’t guaranteed. Asking the right questions up front could be the difference between a role that merely includes night work and one that actually reflects the real costs of working nights.
Disclosure: A version of this post was originally published by Dr. Rob Anderson on KevinMD.